In mental health, the relationship between substance abuse and psychotic disorder is complicated and not always clear. Using drugs is linked to psychotic illnesses, which change how you think, feel, and see things.
Abuse of drugs and mental illnesses affect each other in complicated ways. Psychotic disorders like schizophrenia and schizoaffective disorder can happen at the same time as drug abuse, which can lead to a lot of mental health problems.
Substance abuse and psychotic disorders are complex mental health issues. These diseases can have a major impact on health and require sophisticated treatment. Understanding these illnesses’ impacts and devising treatment and recovery routes requires addressing them.
We promote overall health, integrating physical, mental, and emotional health. Our team at Brightpoint MD provides personalized care to ensure everyone has the assistance they need to succeed.
Understanding Substance Abuse and Psychotic Disorders
Substance abuse psychotic disorders are a spectrum of substance addiction and psychosis. Many kinds of these disorders blur the borders between substance-induced effects and genuine psychotic disorders. They often involve hallucinations, delusions, decreased cognition, and reality distortion.
Substance abuse symptoms and psychotic disorders can range from moderate to severe depending on the drug and susceptibility. Characteristic symptoms include hallucinations, paranoia, disorganized thinking, and separation from reality. These diseases are common, although their effects on mental health vary by substance.
The Complex Relationship: Substance Abuse and Psychotic Disorders
The relationship between Substance abuse psychotic disorders is complex. Substance misuse can worsen psychotic symptoms, and pre-existing psychotic disorders may lead to self-medication. This interconnectedness emphasizes the need to treat both simultaneously.
Data shows the shocking prevalence of psychosis and substance abuse illnesses. Studies show that 40-50% of psychosis patients also have a substance use disorder.
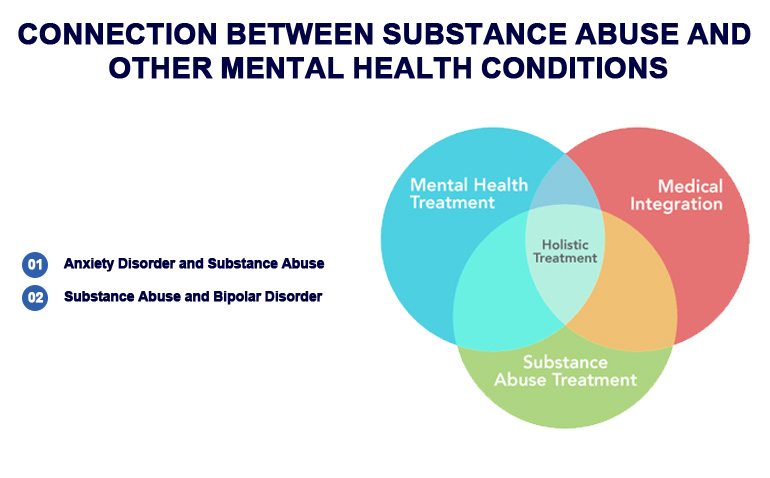
Connection Between Substance Abuse and Other Mental Health Conditions
Anxiety Disorder and Substance Abuse
Mental health issues like anxiety and substance abuse often overlap. They can both worsen each other. Anxiety disorders, which cause excessive concern and fear, may lead to substance usage as a coping technique.
Contrarily, substance addiction increases anxiety. Alcohol and other substances might temporarily relieve stress, but long-term usage can cause panic attacks. Treatment centers in Largo treat anxiety and substance abuse simultaneously through integrated care. Our approach provides non-drug-based coping skills and treats anxiety through therapy and other methods.
Substance Abuse and Bipolar Disorder
Complex relationship between substance misuse and bipolar disorder. Bipolar disorder sufferers may self-medicate with drugs to manage their mood swings and depression. Substance misuse can worsen bipolar disorder symptoms and cause more severe mood episodes.
Treatment Approaches for Substance Abuse psychotic Disorders
Holistic Co-occurring Disorder Treatment
Customized Treatments
We use CBT, DBT, motivational interviewing, and psychopharmacology when needed. These interventions manage symptoms and provide people the tools they need to recover.
Importance of Integrated Treatment for Co-occurring Disorders
Integrated treatment for psychosis and substance abuse disorders has many benefits. These interrelated concerns are addressed simultaneously to provide comprehensive care addressing the problems’ fundamental causes. This reduces relapse, improves treatment outcomes, and promotes long-term recovery.
Co-occurring Disorder Treatment Challenges
Co-occurring disorders are difficult to treat. Specialized care is needed due to symptom complexity, drug interactions, and response variability. Integrated treatment requires interdisciplinary teams to customize tactics for each patient.
Conclusion
Substance abuse psychotic disorders are interconnected, requiring a multifaceted therapeutic approach. Dedicated to holistic care, knows that optimal results need treating both aspects concurrently.
Help is essential to restoring health and well-being. Specialized care for co-occurring disorders gives persons with these complex issues hope. We recommend seeking help for co-occurring substance abuse and psychotic disorders.
Remember, you’re not alone in your healing path. Brightpoint MD offers compassionate, individualized treatment to help you live a healthier, brighter future.
Take the First Step Today
Take that brave step towards comprehensive well-being by seeking information, support, or assistance. Brightpoint MD specializes in treating co-occurring diseases for a happier life.
FAQs
Mental illness and substance abuse may have a tangled relationship. Drug misuse can worsen or exacerbate mental illnesses, and psychotic patients may take drugs to cope.
Different rates of co-occurrence exist, but study demonstrates significant incidence. Studies indicate that many persons with mental conditions also use drugs. This emphasizes the need to address both issues simultaneously.
Drug abuse can worsen psychotic symptoms and increase frequency and severity. Additionally, it can make psychotic diseases harder to diagnose and treat.
Because they are linked, treating co-occurring illnesses is harder than treating other disorders. Some of these problems are figuring out how different treatments interact with each other, dealing with a wide range of symptoms, and coming up with interventions that meet the needs of each person.
Integrated treatment approaches recognize that these conditions are linked and provide complete care that addresses both drug abuse and psychotic symptoms at the same time. The goal of this strategy is to lower the risk of relapse and improve overall outcomes for people who have more than one disorder.

